Gut Microbiota and Cancer Immunotherapy
- haosiqiu2017
- Jan 1, 2025
- 4 min read
Abstract:Gut microbiota, a key component of the human microbiome, profoundly impacts health and disease, including cancer immunotherapy. Immune checkpoint inhibitors like PD-1/PD-L1 drugs revolutionised cancer treatment but are effective in only 15%-20% of patients. Studies reveal that gut microbiota modulates the immune system and affects immunotherapy outcomes. Specific bacteria, such as Coprobacillus cateniformis, enhance drug efficacy by regulating dendritic cells and suppressing the immune checkpoint PD-L2. This discovery highlights new therapeutic strategies, including microbiota-based interventions, cellular therapy, and checkpoint modulation. These advancements offer hope for increasing the efficacy of cancer immunotherapy and benefiting more patients.
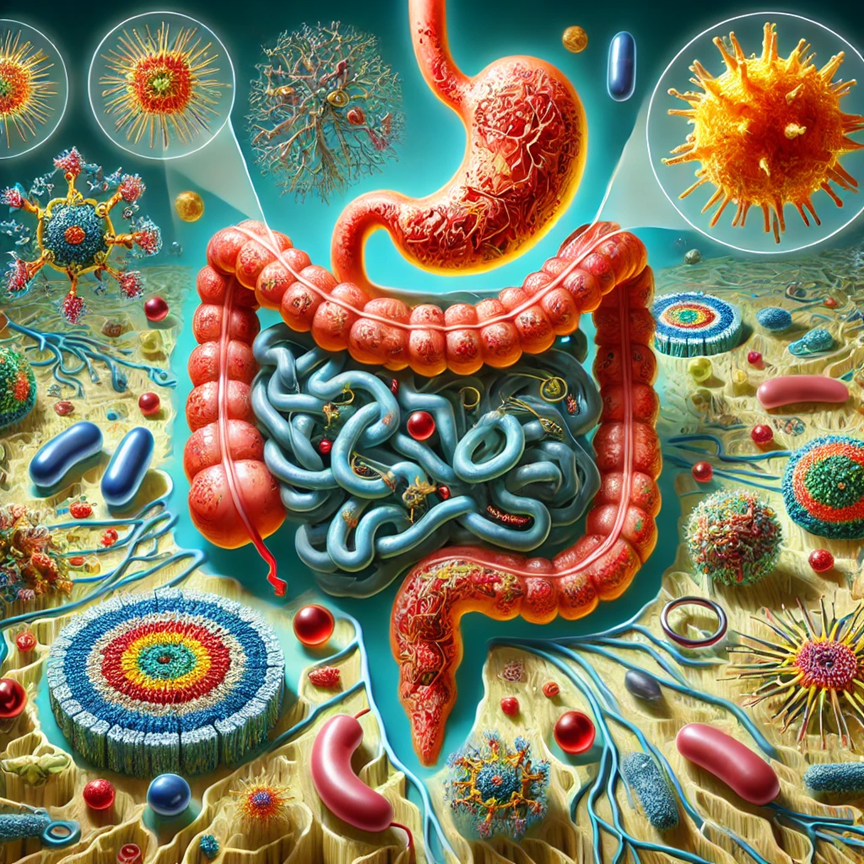
The term "gut microbiota" refers to a significant component of the human microbiome, characterised by its high diversity, vast population, and critical functionality. It represents the collection of bacteria residing in the human gut, contributing to a broader microbiome found in other organs such as the skin, genital tract, and oral cavity. These microorganisms, numbering up to 100 trillion and encompassing around 1,000 species, outnumber human cells in the body .
Recent research highlights the extensive and profound influence of the microbiota on human health and disease. Systemic changes in microbiota composition have been observed in various conditions, including immune, metabolic, neurological disorders, cancer, and cardiovascular diseases. Based on these findings, some researchers regard the microbiota as an essential external organ that supports human physiology.
Cancer immunotherapy, on the other hand, represents the most revolutionary advancement in oncology over the past half-century.
The fundamental principle of immunotherapy is that most mutated cells in the human body, which develop into cancer cells, are identified and eliminated by the immune system, preventing cancer progression. To survive, cancer cells often suppress immune responses by activating specific "immune checkpoints," which serve as brakes on the immune system.
Drugs targeting these immune checkpoints have been developed to restore immune activity and enable the immune system to attack cancer cells effectively. For example, PD-1/PD-L1 is a well-known immune checkpoint pathway where cancer cells express PD-L1 to bind to PD-1 on T cells, inhibiting their function. Drugs targeting PD-1 (e.g., Nivolumab, Pembrolizumab) or PD-L1 (e.g., Atezolizumab, Durvalumab) have shown efficacy in treating various cancers .
At first glance, there seems to be no direct connection between gut microbiota and cancer immunotherapy. However, in 2015, researchers demonstrated in mouse models that the efficacy of cancer immunotherapy depends on the presence of microbiota. Germ-free mice or those treated with antibiotics to deplete gut bacteria showed no response to immune checkpoint inhibitors .
By 2018, similar findings were confirmed in humans. For melanoma patients, the composition of gut microbiota correlated with their response to immunotherapy. Moreover, antibiotic use was associated with reduced efficacy of immune checkpoint inhibitors in cancer patients .
How Gut Microbiota Influences Cancer Immunotherapy
The logical connection is that gut microbiota regulates immune system development and function, which directly impacts the effectiveness of cancer immunotherapy. However, the specific mechanisms remained elusive.
Researchers have started exploring strategies such as fecal microbiota transplantation (FMT) from patients who respond well to immunotherapy to non-responders, yielding some positive results . Yet, this approach is cumbersome and carries safety risks, such as transferring pathogenic or antibiotic-resistant bacteria.
A more precise strategy involves understanding which microbial components influence immune cells and through what mechanisms. This knowledge could lead to the development of targeted drugs to enhance immunotherapy efficacy without relying on the microbiota.
A Breakthrough Study: New Pathways in Cancer Treatment
On May 11, 2023, a groundbreaking study published in Nature made significant progress in elucidating these mechanisms. Led by researchers at Harvard Medical School, including pioneers Gordon Freeman, Arlene Sharpe, and Dennis Kasper, the study uncovered how gut microbiota influences a lesser-known immune checkpoint pathway, PD-L2/RGMb, which competes with the PD-L1/PD-1 axis .
Key Findings:
Microbiota Dependency: In a mouse model with colon cancer cells (MC38), germ-free mice or those with depleted gut microbiota showed no response to PD-L1 antibody treatment. Restoring microbiota via transplantation from healthy donors reinstated the therapeutic response.
Role of PD-L2: Mice lacking gut microbiota exhibited elevated PD-L2 expression, which suppressed immune function. Adding PD-L2 antibodies alongside PD-L1 inhibitors restored anti-tumour efficacy, even in germ-free mice.
Human Validation: Transplanting microbiota from non-responding cancer patients into germ-free mice resulted in resistance to PD-L1 inhibitors. Adding PD-L2 antibodies reversed this resistance, highlighting its clinical relevance.
Critical Bacteria Identified: Researchers identified Coprobacillus cateniformis as a key bacterium. Mice lacking this bacterium failed to respond to immunotherapy, while its introduction restored treatment efficacy. This bacterium modulates dendritic cells by suppressing PD-L2 expression, thereby enhancing immune activation.
Dendritic Cells and PD-L2: Dendritic cells serve as a bridge between microbiota and the immune system. Gut bacteria like C. cateniformis inhibit PD-L2 expression in dendritic cells, reactivating their function and boosting the immune response.

Implications for Cancer Treatment
This study establishes a credible causal link between gut microbiota and cancer immunotherapy efficacy. It highlights dendritic cells and PD-L2 as pivotal mediators. These findings suggest new therapeutic strategies:
Microbiota-Based Approaches: Transplantation of beneficial bacteria or using bacterial extracts to stimulate immune cells.
Cellular Therapy: Culturing and stimulating dendritic cells ex vivo before reinfusion into patients, potentially enhanced by bacterial extracts or PD-L2 gene editing.
Checkpoint Modulation: Targeting the PD-L2/RGMb axis with drugs to improve immune activity and tumour eradication.
A New Frontier in Oncology
Cancer immunotherapy has transformed oncology, offering hope to patients unresponsive to traditional treatments. However, its efficacy is limited to approximately 15%-20% of patients [16]. Expanding the scope of responsive patients remains a critical challenge.
Exploring microbiota-immune system interactions offers one promising avenue. Combining immunotherapy with other approaches, such as chemotherapy, radiotherapy, cytokine therapy, or tumour antigen discovery, may pave the way for more comprehensive solutions .
By deepening our understanding of these mechanisms, we can aspire to turn all “cold” tumours into “hot” ones, enabling every cancer patient to benefit from these revolutionary therapies.





Comments